Vivian Y. Lin, Niroop Kaza, Susan E. Birket, Harrison Kim, Lloyd J. Edwards, Jennifer LaFontaine, Linbo Liu, Marina Mazur, Stephen A. Byzek, Justin Hanes, Guillermo J. Tearney, S. Vamsee Raju, Steven M. Rowe
European Respiratory Journal 2020 55: 1900419; DOI: 10.1183/13993003.00419-2019
Abstract
The mechanisms by which cigarette smoking impairs airway mucus clearance are not well understood. We recently established a ferret model of cigarette smoke-induced chronic obstructive pulmonary disease (COPD) exhibiting chronic bronchitis. We investigated the effects of cigarette smoke on mucociliary transport (MCT).
Adult ferrets were exposed to cigarette smoke for 6 months, with in vivo mucociliary clearance measured by technetium-labelled DTPA retention. Excised tracheae were imaged with micro-optical coherence tomography. Mucus changes in primary human airway epithelial cells and ex vivo ferret airways were assessed by histology and particle tracking microrheology. Linear mixed models for repeated measures identified key determinants of MCT.
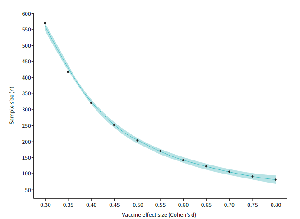
Compared to air controls, cigarette smoke-exposed ferrets exhibited mucus hypersecretion, delayed mucociliary clearance (−89.0%, p<0.01) and impaired tracheal MCT (−29.4%, p<0.05). Cholinergic stimulus augmented airway surface liquid (ASL) depth (5.8±0.3 to 7.3±0.6 µm, p<0.0001) and restored MCT (6.8±0.8 to 12.9±1.2 mm·min−1, p<0.0001). Mixed model analysis controlling for covariates indicated smoking exposure, mucus hydration (ASL) and ciliary beat frequency were important predictors of MCT. Ferret mucus was hyperviscous following smoke exposure in vivo or in vitro, and contributed to diminished MCT. Primary cells from smokers with and without COPD recapitulated these findings, which persisted despite the absence of continued smoke exposure.
Cigarette smoke impairs MCT by inducing airway dehydration and increased mucus viscosity, and can be partially abrogated by cholinergic secretion of fluid secretion. These data elucidate the detrimental effects of cigarette smoke exposure on mucus clearance and suggest additional avenues for therapeutic intervention.
Mucus abnormalities impact COPD airway clearance http://bit.ly/2VEhFjd
Footnotes
-
This article has an editorial commentary: https://doi.org/10.1183/13993003.02473-2019
-
This article has supplementary material available from erj.ersjournals.com
-
Author contributions: V.Y. Lin performed rheologic measurement of mucus samples, and analysed the data. V.Y. Lin and S.E. Birket optimised the tracheal explant imaging protocol, performed µOCT imaging of airway samples, and analysed the data. S.V. Raju and H. Kim performed in vivo MCC assays and analysed the resulting images. S.A. Byzek performed in vivo smoke exposures. S.V. Raju, S.A. Byzek and N. Kaza performed animal necropsies for trachea studies. L.J. Edwards performed statistical modelling of µOCT data. J. LaFontaine performed histologic analysis of bronchial and lung tissue. S.A. Byzek measured TPM output throughout exposure studies. M. Mazur harvested and grew cells from human donor tissue for primary cell culture. J. Hanes provided fluorescent nanoparticles and expertise for particle tracking experiments. G.J. Tearney developed µOCT technology and all related analytical methods, and provided technical support and expertise. V.Y. Lin, S.E. Birket, S.V. Raju and S.M. Rowe contributed to experimental design and data interpretation. V.Y. Lin and S.M. Rowe wrote the manuscript, which was reviewed by N. Kaza, S.E. Birket, S.V. Raju, H. Kim, M. Mazur, S.A. Byzek, J. Hanes and G.J. Tearney.
-
Support statement: This study was financially supported by the National Institutes of Health (NIH grants P30DK072482, R35HL135816 and F31HL134225), and the Flight Attendant Medical Research Institute. Funding information for this article has been deposited with the Crossref Funder Registry.
-
Conflict of interest: V.Y. Lin has nothing to disclose.
-
Conflict of interest: N. Kaza has nothing to disclose.
-
Conflict of interest: S.E. Birket has nothing to disclose.
-
Conflict of interest: H. Kim has nothing to disclose.
-
Conflict of interest: L.J. Edwards has nothing to disclose.
-
Conflict of interest: J. LaFontaine has nothing to disclose.
-
Conflict of interest: L. Liu has a patent “Method for functional investigation of respiratory airways and other ciliated tissues using µOCT” pending.
-
Conflict of interest: M. Mazur has nothing to disclose.
-
Conflict of interest: S.A. Byzek has nothing to disclose.
-
Conflict of interest: J. Hanes is founder and owner of company stock (which is subject to certain rules and restrictions under Johns Hopkins University policy) of GrayBug Vision, Inc., and Kala Pharmaceuticals, Inc., outside the submitted work.
-
Conflict of interest: G.J. Tearney has patents 14/240,938 and 12826303.5 pending.
-
Conflict of interest: S.V. Raju has nothing to disclose.
-
Conflict of interest: S.M. Rowe reports grants from Bayer, Forest Research Institute, AstraZeneca, N30/Nivalis, Novartis, Galapagos/AbbVie, Proteostasis, PTC Therapeutics and Eloxx, grants and personal fees for consultancy from Celtaxsys, personal fees for consultancy and advisory board work and in kind support for clinical trial work from Vertex Pharmaceuticals Incorporated, personal fees for consultancy from Bayer and Novartis, outside the submitted work; and has a patent “Use of OCT as a diagnostic modality for diseases of mucus clearance” issued.
- Received February 28, 2019.
- Accepted October 9, 2019.
- Copyright ©ERS 2020